Maps distort reality, and so do our health metrics.
Traditional world maps like the Mercator projection distort the relative size of countries, magnifying the global north while shrinking equatorial nations. These visual distortions subtly shape our perceptions of power, influence, and importance.
But cartography isn’t the only field influenced by outdated perspectives.
Health systems, too, are governed by legacy mental models that prioritise dominant but narrow metrics: budget size, hospital capacity, and wait times. These don’t reflect what truly matters: access, equity, continuity, and outcomes.
If we’re serious about delivering universal, people-centred care, we must recentre how we evaluate, manage, and reform health systems.

This visual comparison between Australia, North America, the UK, and Russia corrects the distortions of traditional maps.
Big budgets don’t guarantee big results
Some of the most successful and agile health reforms in the past two decades have come not from large, well-resourced nations but from smaller ones. Countries like Estonia and Singapore have turned fiscal constraints and demographic pressure into drivers of innovation.
In contrast, large systems such as England’s NHS have sometimes struggled to translate investment into consistent patient experiences. Systemic inertia, fragmented governance, and political churn often stand in the way of real reform.
A 30-country comparative study confirmed what many policymakers suspect but rarely say aloud: there’s no one-size-fits-all solution to health reform. Context matters.
Local governance structures, public trust, leadership continuity, and adaptive policy design are often more impactful than sheer health spend.
Delivery, not strategy, Is the secret to health reform
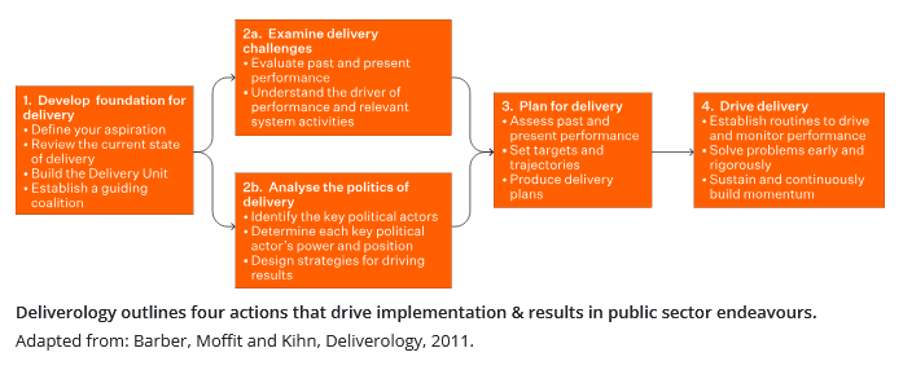
The most overlooked factor in successful reform isn’t vision; it’s execution. Drawing from the UK’s Deliveryology framework, four critical levers underpin high-performing reforms:
- Building a foundation for delivery;
- Understanding performance drivers;
- Crafting and executing delivery plans;
- Sustaining implementation via feedback loops and political will
Too often, bold strategies falter not from lack of ambition but from the absence of machinery to convert ideas into real-world impact.
Prevention isn’t optional, it’s essential
Do voters really want more spending on prevention, especially if it means less on treatment? Surprisingly, yes. If prevention is paired with access, equity, and trust in the system.
Prevention is not a moral luxury. It’s a clinical and fiscal necessity. Innovations like polygenic risk scores and GLP-1 therapies show promise in reducing chronic illness, but their benefits must be broadly accessible, not monopolised by the few.
Related
A prevention-first approach will only work if it’s equitable and politically supported. Left to market forces alone, it risks becoming another vehicle for inequality.
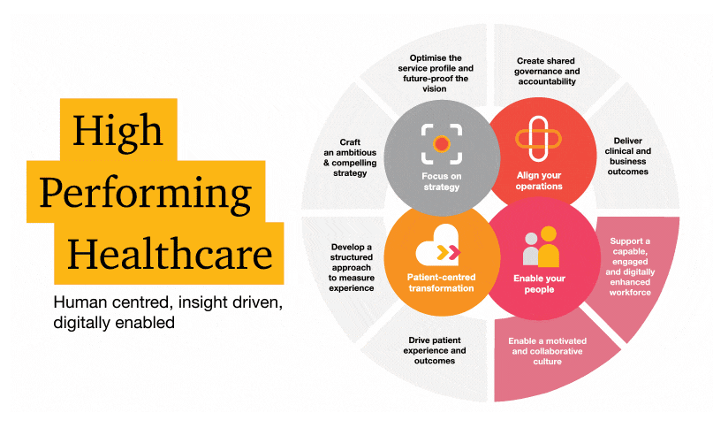
This framework highlights what matters most: experiences and outcomes for patients, staff, and communities rather than just the system’s inputs.
What truly drives health system performance?
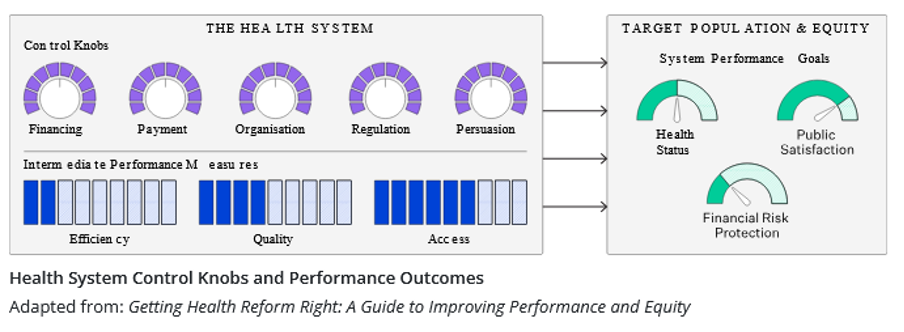
This framework illustrates how policy levers or “control knobs” affect performance outcomes. True system transformation requires aligning these levers with final goals such as equity and improved health outcomes, not just efficiency metrics.
Crisis as catalyst: will we seize the moment?
History shows us that crises often create windows for meaningful reform. [Covid], like past financial shocks, cracked open the system’s rigid structures.
However, whether that window leads to transformation or retrenchment depends on leadership. Reform isn’t inevitable; it must be actively chosen, shaped, and sustained.
It’s time to recentre what matters most
We need to recentre not just our maps, but our mindsets.
Not just our metrics but also our values.
Let’s prioritise:
- Equity over hierarchy;
- Patient voices over institutional volume;
- Health outcomes over traditional orthodoxy.
Only then can we build systems truly fit for the people they serve.
Tom Varghese is global product marketing and growth manager at Orion Health. This article was first published by Orion Health. Read the original article here.




