General use items will stay on the Prescribed List. The only ones not happy are the private health insurers.
The federal government has reversed the Morrison government’s 2021 decision to remove general use items from the list of medical products, devices and prostheses that private health insurers must pay for.
The plan was due to come into effect on 1 July this year, but Health Minister Mark Butler announced today that the Albanese government has reversed that decision.
“The government has listened to the concerns about the pressure removing general use items would have caused and decided that this achieves the best outcome for patients,” said Mr Butler.
“To maintain access to quality healthcare and to provide certainty to private hospitals and patients, the cost of these common surgery items will continue to be funded through the Prescribed List.”
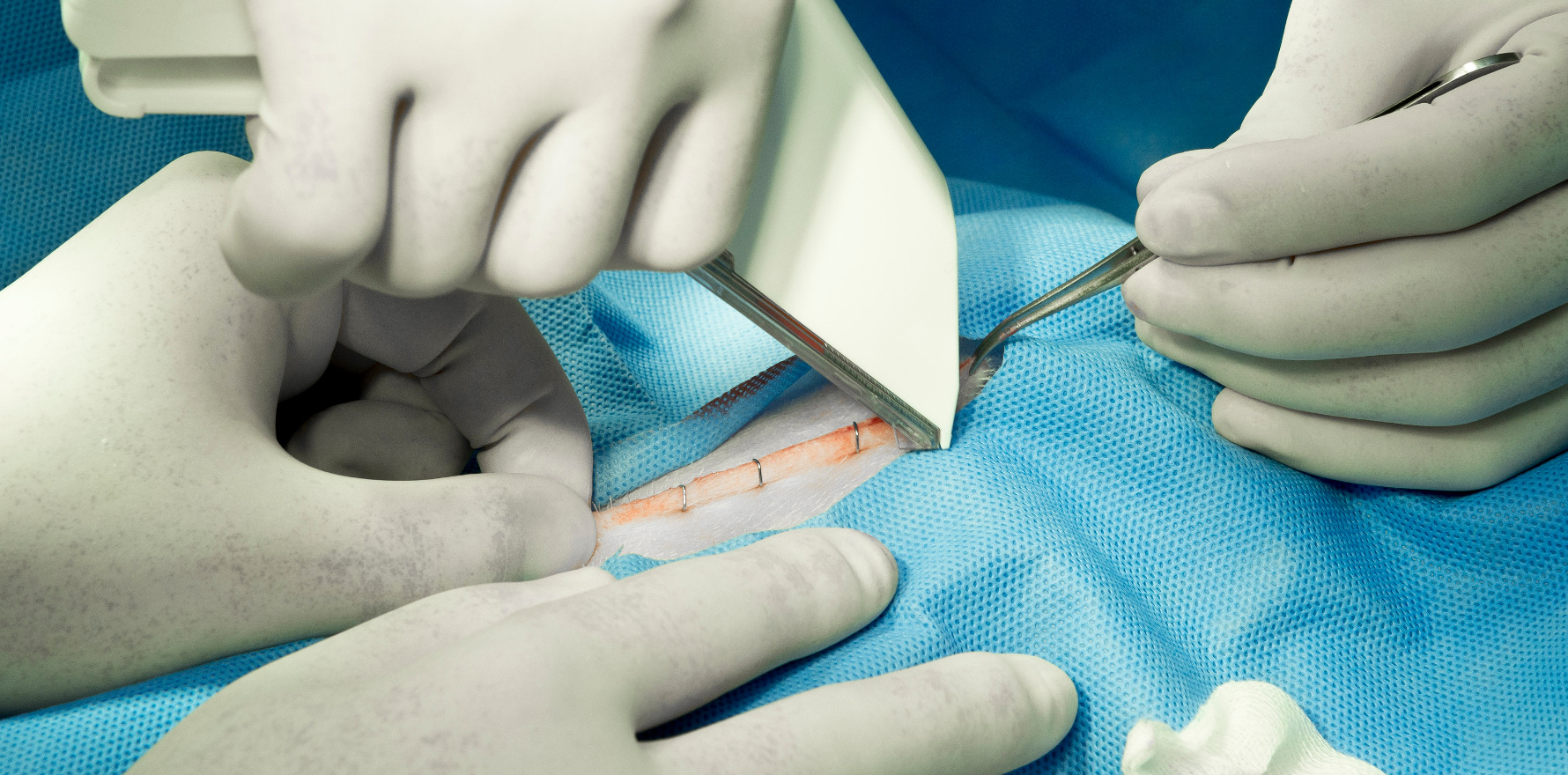
General use items cover a wide range of items commonly used in surgeries, like staples, sutures, and glues. Reforms to reduce the prices of general use items have already been estimated to save over $78 million, according to the Department of Health and Aged Care, putting downward pressure on private health insurance premiums.
The removal of these items from the Prescribed List raised questions over whether those costs would now be carried by patients with private insurance through higher out-of-pocket fees, or private hospitals.
So far, the only people unhappy with today’s decision are the private health insurers.
Not surprisingly, Dr Rachel David, CEO of Private Healthcare Australia, which represents 98% of the health insurance sector, said the decision risked “driving up premiums, paying too much for common medical supplies” and wasting “limited funding that could be better spent delivering timely, effective health services”.
“The decision to wind back the planned removal of general use items … is likely to impact the cost of private health insurance premiums for 15 million Australians,” said Dr David.
“Health funds are extremely disappointed private hospitals have collectively rejected offers for fairer pricing of hundreds of medical supplies as part of the federal government’s reforms to the Prescribed List of Medical Devices and Human Tissue (formerly known as the Prosthesis List).”
The PHA has called for the following measures to take effect from 1 July to reduce pressure on health premiums:
- An enforceable Code of Conduct to prevent upselling of general use items by sales reps in operating theatres, and mandatory reporting of any kickbacks paid to hospitals or doctors. Whistleblowers have exposed these practices occurring in hospitals; and
- A range of measures to remove incentives for the overselling and overpricing of commonly used medical items.
“Over the past year, all health funds offered to pay private hospitals new funding arrangements for hundreds of general use items used in surgery, such as sponges, staples and catheters, which should never have been on the Prescribed List (PL) in the first place,” said Dr David.
The Morrison government commissioned EY to produce a report in 2020, which found that paying for every single individual item was inefficient and incentivised hospitals to use more devices, the PHA said.
“The reforms to the PL are designed to create a more competitive market for medical supplies in the private health sector so health funds do not have to pay exorbitant prices for common medical supplies via a list of government-set prices that have not been the subject of negotiation with payers, including health funds,” said Dr David.
She said “these higher costs are subsequently borne by consumers”.
“While health funds understand private hospitals, like all sectors, have been under pressure due to inflation and workforce shortages, the solution does not lie in health funds paying inflated prices for common medical supplies that could be purchased at lower prices,” she said.
“Health funds are doing everything they can to ensure their members do not pay more than they have to for health insurance during a cost-of-living crisis and we will work to ensure proper safeguards are introduced to protect against inflation and its impact on premiums.”
Meanwhile, the Australian Private Hospitals Association “welcomed” the reversal.
Michael Roff, outgoing CEO of the APHA, said removing GUIs from the list would have made some surgeries “untenable” for private hospitals.
“Procedures like bariatric surgery, knee replacements, and cardiothoracic surgery would have been at risk in the private sector, potentially leading to increased demand on overstretched public hospitals,” said Mr Roff.
“The health insurance sector had not been able to devise a sustainable funding model for GUIs, which would have left private hospitals managing increased costs at a time they could least afford it.
“Despite a range of proposals from different health insurance companies, none offered a viable alternative funding model with all of them shifting financial risk onto private hospitals. Potentially, this could have added $250 million in costs to the private hospital sector.
“We are grateful the minister has listened to our representations.”
Catholic Health Australia was also pleased, saying the decision was a “common-sense, patient-focused approach”.
“Private hospital patients around the country can today breathe a sigh of relief, knowing their health insurer will still be required to cover critical surgical items,” said CHA CEO Jason Kara.
“The government’s commitment to upholding the funding for general use items is a crucial decision that will help ensure no patient is left behind, especially women and those in regional communities.
“The government has stood up to lobbying from some private health insurers,” he said.
“We thank the government for its close consultation with the Catholic hospital sector and commitment to ensuring there are no adverse impacts on patients or unintended consequences from these reforms.”