Healthcare marketing platforms are only just getting going, which means the government (and GPs) need a better plan.
It’s easy to hate the fast-growing health marketing platform Eucalyptus (Pilot, Juniper and other brands).
If you ever met the founders you’d likely find it even easier. They are to healthcare what Mark Zuckerberg, Sergey Brin, Larry Page and Elon Musk have been to the internet and social media.
All of these guys – all white blokes, just saying – talked a big game at the start of their ventures about stuff like creating community, empowering people, bringing people together and connecting the world.
Really, it was always about power and money.
Those promises turned out to be one of the all-time great bait-and-switches for our data and money.
The kind folk at Euclyptus love to paint themselves as creative, young, good guys breaking down conservative barriers created by generations of tradition in medicine with innovation and modern, empathetic thinking.
Eucalyptus promises to democratise health by using technology to make it accessible to the masses. “We deliver healthcare that puts patients first,” their actual website copy says. “As a global telehealth provider, we’re building a safe, effective and accessible future for medicine.”
None of this real.
Their flagship product costs over $400 per month, which kills the accessibility line from the get-go. They’ll tell you it’s too hard to see a GP and that they are overcoming that issue as well. Hmmm – mixed billing is becoming a new obstacle to access but I’ve yet to see a GP adding $400 to their consult, or a patient who would pay $400 up front to see one, so that line is rubbish as well.
They aren’t providing care. They are selling product en masse and doing just enough checking around the process of supply (medical oversight) to not kill anyone – something that could easily happen operating at such high throughput if you aren’t careful enough.
Their innovation and modern thinking is actually just repurposing some long established tech platform marketing principles and strategy – Amazon, Google, Apple, Uber and so on led the way – for the low-hanging fruit in health.
So they’re not the smart, innovative, likeable folk they like to present themselves as.
But here’s the thing. Like the big global tech platform plays, these new emerging health platform marketing plays are never going away.
They’re just going to get a lot bigger from here.
Fast, telehealth-driven, single-indication medicine and health provision has hardly even started in Australia.
Amazon isn’t really here in health yet but it is prepping in earnest and Wesfarmers, Woolworths et al only have their toes in the water so far.
With the data these groups have on everyone, and some of the upstream companies they’ve already acquired – a giant pharmacy wholesaler in the case of Wesfarmers – what Eucalyptus is doing so far might turn out to be pretty tame.
The other reason we now know these new platform plays aren’t going anywhere is that a reasonably large demographic of patients – cashed up, young, often without a regular GP –love the convenience and the impersonal nature of these platform services.
How do GPs compete with these monsters? They don’t because they can’t.
GPs don’t do what these platforms do. If they started to, the healthcare system would be in a lot of trouble. Neither would the majority of GPs or GP practices want to even try, because that’s not what they signed up for when they decided to do medicine.
In addition, at this stage of the development of these companies, investors are happy to lose a lot of money to build a market. You can’t beat someone who can afford to operate at a loss for a few years.
This isn’t to say the government or GPs should just ignore these new companies.
If GP practices keep doing what they’ve always been doing, these new providers will skim patients and margin. Since even a good practice runs on reasonably slim margins – 5% is a figure bandied around by the analysts – and taking into account all the other emerging cost and operational issues GP practices are currently facing, this might just be that straw on a certain camel’s back.
Dr Max Mollekopf is an interesting, creative and outspoken GP and practice owner who is all over this dynamic and has a pretty good line on how owners can approach this emerging problem.
He has accepted that you can’t beat them and you wouldn’t want to even try, so you need to work harder on what you have in your business model that these new platforms don’t have.
It’s marketing 101 and it turns out that GPs have a pretty unique value proposition that, with not too much tweaking, might create a surprisingly brighter future than many people are forecasting.
“As a GP running a small community practice I’m not worried about Amazon or Wesfarmers Health coming into the primary care space,” Mollekopf says on a recent Linked In post on the subject.
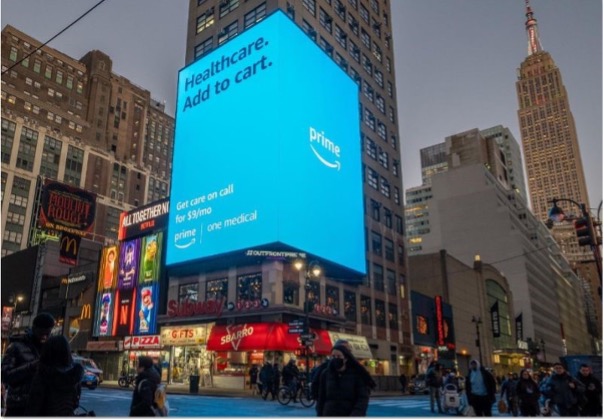
Pointing to the ad below for providers now owned by Amazon in the US, Mollekopf points out that quality and longitudinal care is just not a part of their offering.
“In my world I service consumers who value quality. I see patients who want someone who knows them, knows their family and provides more than a prescriber number for hire. I’m always working to enhance my technology stack so I can move with my younger patients but that’s all about being a modern version of general practice. There will always be patients in our community who value community-driven quality care and that’s where GPs like myself and my colleagues should be continuing to focus their energy.”
By the by, if you were to go to see Dr Max and get Ozempic off-label to help you lose weight, it would cost you about $190 a month (including drug and a mixed billing fee), not $400, and you’d have all that actual love and caring and long-term security about your overall health to go with it – which is Dr Max’s competitive advantage against Eucalyptus in a nutshell.
If you stayed with Dr Max for 20 years, your saving would be in the realms of $40,000 to $50,000 just on the weight loss part of the relationship.
As with Uber and AI, there aren’t enough guardrails in place to manage these fast-growing tech behemoths.
For starters, they exist outside what was once the system – Medicare – so they can do a lot of things that wouldn’t normally be acceptable.
For example, buying semaglutide sodium in bulk from a supplier you aren’t prepared to name, to compound an Ozempic substitute that is unregulated and untested by anyone that the government recognises as qualified for the job, to sell to your customers while you can’t get the good stuff – Ozempic, which has been rigorously tested for safety through the FDA and TGA.
It says a lot about how these companies view the traditional health system regulators like the TGA, the DoHAC, AHPRA and the Medical Board of Australia.
Semaglutide sodium, which is what Eucalyptus (and similar single-indication marketing platforms) are using as a replacement product for their patients, seems to have red flags all over it from a safety risk and therefore brand reputation perspective:
- It doesn’t meet standards for compounding law in the US, according to the Federal Drug Administration, which wrote to compounding pharmacy associations saying: “We are not aware of any basis for compounding a drug using these semaglutide salts that would meet federal law requirements” and has issued adverse drug reaction alerts around its use already;
- The TGA has similar concerns and issued its own warning in December that compounded semaglutide-like products were “unapproved” therapeutic goods that had not been evaluated for safety, quality and efficacy and should be only “reserved for exceptional clinical circumstances”; and
- No one creating the substitution is prepared to name the manufacturers of the semaglutide sodium, almost certainly because those suppliers are in India or China. These two countries supply the majority of raw materials for most pharmaceutical manufacturers around the world, but that particular supply chain is very tightly regulated, governed and monitored for safety. This supply of raw material is being kept deliberately opaque by Eucalyptus and the compounders, which creates a very obvious safety issue.
Why is Eucalyptus taking what looks like such a big potential risk to its brand and reputation?
Money, mostly (what else?).
At the more than $400 per month they are charging their customers, if they lose anyone they’ve spent good money acquiring in the last year or so, they might be losing up to $100,000 per customer over that customer’s life – maybe even more.
Eucalyptus’s founder Tim Doyle says the company has helped 50,000 people lose weight already. If the Ozempic shortage, which is predicted to go on for another year at least, caused it to lose just 20% of this number, they’d be forgoing $1 billion in future revenues. And that’s not counting all the new customers they’d be looking to acquire during the shortage period.
Ozempic has supercharged the Eucalyptus business. Stopping supply at this point of its growth cycle is not an option.
From a business and investor perspective, without continuity of supply, Eucalyptus might well be in trouble. It looked like it was heading for trouble before it stumbled into the Ozempic phenomenon.
Eucalyptus is madly rushing to get enough market position and brand solidarity before the real behemoths of future platform health provision – Amazon, Wesfarmers, Woolworths and who knows who else from overseas – get their mojo on here. If it is well enough established in time it will make more sense to buy Eucalyptus than squash it with their endless reserves of capital.
We shouldn’t be surprised at Eucalyptus’s disregard of the current regulatory regime of health, or its neat dancing through all the loopholes that exist in a system focused on Medicare, where the government pays most of the time.
It’s all from the global technology platform playbook. It’s no different to how Uber approached regulation and government in growing.
Eucalyptus knows it has a window in which government takes forever to understand, makes a few false starts, does a couple of expert reviews, navigates the next election, and finally does something about what is going on.
One reason why government would struggle to rein in companies like Eucalyptus in health, even if it was suddenly magically agile and all knowing, is that it’s entirely unclear whether platforms like Eucalyptus are going to be a good or a bad thing in the end for patients and the system.
Okay, they care more about money than about patients. But that doesn’t mean that what they’re doing won’t have some place in a more efficient system into the future.
Take Eucalyptus’s major growth engine product: weight loss.
The con of treating masses of patients for obesity and pretty much nothing else is that obesity is associated with a multitude of other potential chronic issues that likely need more sophisticated longitudinal care. If they treat just one condition en masse like Eucalyptus is doing, might these companies unwittingly drag patients away from the care they really need: more sophisticated multi-indication longitudinal care for all those comorbidities associated with obesity?
And might that end up costing the system way too much in additional burden on managing chronic care in the public system?
On the other hand, if they end up reaching enough people and treat them effectively for obesity, that could avoid the emergence of some of those morbidities in a lot of patients.
It might even save the public system some money.
Of course, we’re talking only about a relatively rich demographic – you’ll need a spare $5k a year to stay with Eucalyptus. Maybe these platform providers will relieve the system of some richer people who might normally have gone to a GP or hospital and incurred public expense but have the money and desire to just pay to avoid all that.
We don’t like Eucalyptus et al hiding their grasping natures behind palaver about access and patient wellbeing. But there is nothing yet to say definitively if they will end up being good or bad for the overall health of the nation.
Health is not business. It’s a core fundamental of government service to its citizens and the second most expensive part of running government to defence (should be first, but hey).
If health marketing platforms were obviously bad for the system and patients the government would have every right to step in quickly and regulate them out of the picture.
But we don’t know that.
There is one thing government must do and quickly: regulate or legislate so that the data being generated by these newcomers is available to the government, so it can plan properly.
Today, while the government can largely track data and trends in the system it set up in the old paradigm – Medicare – all the data on patients and consults being generated by these new platforms and private providers is largely invisible to them.
Planning without this data is planning with one arm tied behind your back.
Every health transaction that exists outside of Medicare should be visible to the government so it can watch over the whole system. Healthcare is way too costly and too important for the government and patients not to have proper visibility over the big picture.
Creating such legislation might be lot easier than many might think.
The government has promised to legislate this year to make pathology and radiology companies share their data seamlessly in real time through the My Health Record. Currently path labs hold back this data to protect their current revenue models. Pathology companies are a much bigger political headache to lean into than the healthtech sector. If you’re going to annoy the big nasty dog may as well reign in all the puppies with them.
In addition, the government has promised to create a system where all health data can be shared securely between providers and patients in real time. It’s calling that program “sharing by default”.
It seems obvious now that that needs to include everyone doing healthcare transactions, not just those in the traditional Medicare ecosystem.
That means that everyone currently outside the purview of government – the various Eucalyptus brand platforms, all the new emerging private telehealth providers, and any other private provider transacting outside of Medicare, must be brought into the tent and quickly.
If we do that we can measure what is actually going on with patients who are opting to use these new emerging platforms and whether it is good or bad for the system.
We can plan healthcare properly into the future and manage far better for patients.
Something that very clearly Eucalyptus is actually not committed to doing.
If you want to talk to some doctors who work for Eucalyptus, Mosh and other emerging platforms, or Dr Mollekopf, come to Burning GP on June 14 at the Mantra on Salt Beach at Kingscliff, northern NSW, where we will be debating these and a lot of other bleeding-edge issues for the GP community. Find the program and tickets here and use the discount code BGP10 to get 10% off any ticket combination for the next two weeks.



