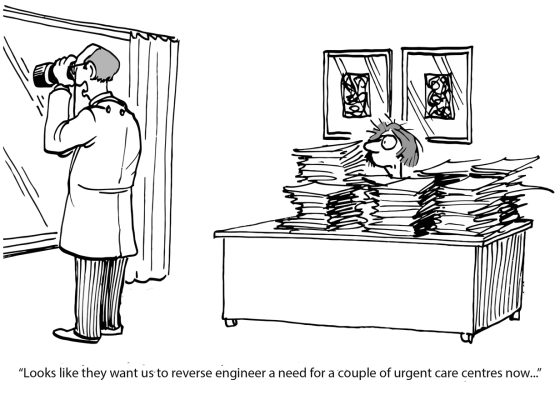
If we want different results – actual improvements in health and equity – we can't just ask for them. We must change the rules. We must redesign commissioning.
Why do hospitals consistently buy workflow efficiency over patient impact?
It’s not a moral failing. It’s a rational response to the rules we’ve set.
We have a commissioning problem. We measure, fund, and manage for throughput, so the entire system optimises for it.
This creates the very symptom Kevin McDonnell described in his great post on LinkedIn: HealthTech founders learn the hard way that “Moral impact earns admiration; operational impact earns adoption”.
If we want different results – actual improvements in health and equity – we can’t just ask for them. We must change the rules. We must redesign commissioning.
Here’s the new playbook:
1. Start with the population.
Don’t start with the service, the facility, or the tech. Use data to explicitly name the target cohorts, their holistic needs (clinical and social), and the specific equity gaps the provider is being paid to close.
2. Measure, drive and pay.
Shift performance management and funding signals to a balanced set of indicators. Include cohort-level needs, costs, activity, experiences (PREMs), outcomes (PROMs), and equity goals. This reframes throughput as necessary, but not sufficient.
Related
3. Operational fit is baseline.
Stop treating workflow savings as the main prize. Operational efficiency, EHR integration, and clinician usability are the “entry ticket”.
The hallmark of outstanding quality is the proven ability to improve outcomes and address inequities for defined population groups.
Jay Rebbeck is CEO of Rebbeck, working with public-sector leaders to create brilliant services and thriving communities through commissioning excellence.
This article was originally published on LinkedIn. Read the original here.