A collaborative localised approach spearheaded by the Murray Primary Health Network.
The completion of a local health needs assessment led to key health services in the Lower Hume region collaborating to form a new primary mental health service.
Service delivery, communication and the patient experience have all been significantly improved by an eReferral system that has integrated and embedded workflows.
In 2024, Murray Primary Health Network (PHN) completed a localised mental health needs assessment (HNA) that identified service gaps in Mitchell and Murrindindi local government areas (LGAs) in Central Victoria.
These included limited local access and long wait times for mental health services beyond general practice settings.
There was also significant confusion navigating the system and fragmented, unclear communication structures, resulting in community members unable to access services for primary mental health support.
These needs were worsened by the rural location and lack of mental health service supply, compared with other parts of the Murray PHN region.
To address this service need, Murray PHN supported a consortium approach to the establishment of the Lower Hume Primary Mental Health Service, created through a co-design process.
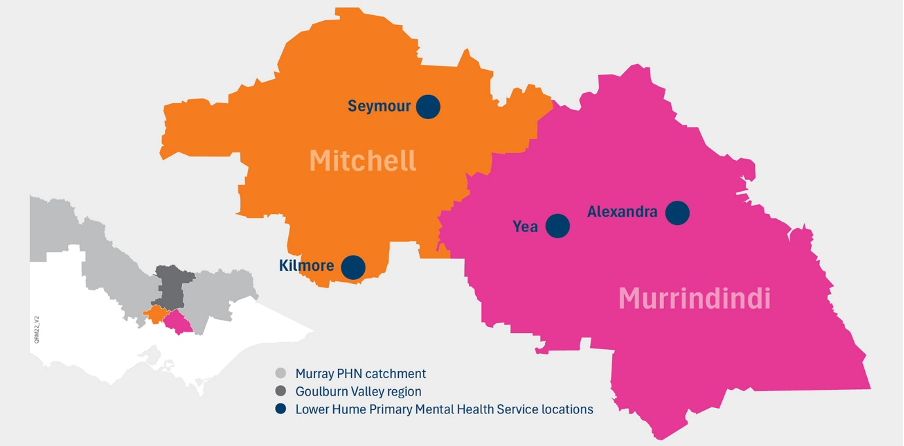
The service is led by Yea & District Memorial Hospital in partnership with Alexandra District Health, Seymour Health, Northern Health and Goulburn Valley Health. It helps to connect people living in Mitchell and Murrindindi LGAs with primary mental health clinicians based in Yea, Alexandra, Seymour and Kilmore.
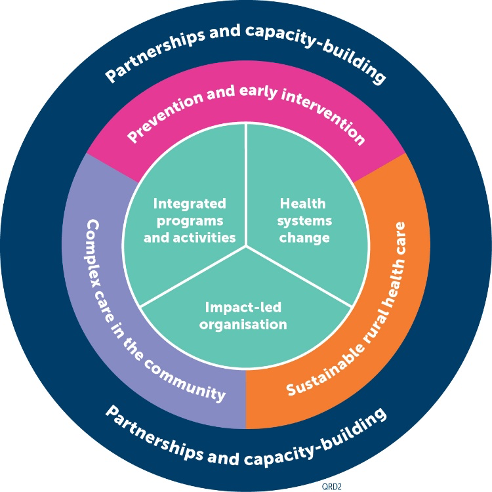
The success of the subregional model has been secured by:
- co-designing and commissioning a clinical service to address identified gaps in primary mental health service supply;
- reducing duplicated and fragmented systems using digital health solutions and agreed standard operating procedures, including a single point of access; and
- enhancing access to evidence-based primary mental health services and communication between referrers and service providers, with the introduction of an eReferral system and the integration of clinical assessment, management and referral pathways.
So far, the program has seen the launch of a new locally based service with agreed standard operating procedures, establishment of new eReferral receiver and sender sites, with one single entry point that refers to receiver sites, and the onboarding of seven new general practice sender sites.
Murray PHN’s digital health strategy for eReferral includes a planned expansion. Currently, 122 general practices across the Murray PHN region are actively using SeNT to electronically refer patients to services across 18 receiver sites (with more scheduled for integration).

Murray PHN CEO Matt Jones (pictured above) said that partnerships were at the heart of the Lower Hume Primary Mental Health Service’s purpose.
“Effective collaboration leads to improved population health outcomes and a more robust and sustainable primary care system,” Mr Jones said.
“We know that access to healthcare can be more difficult in rural and regional areas, but when we work together to support our communities to manage and improve their health and wellbeing, people get the care they need closer to home and fewer people need to seek acute healthcare.”
Murray PHN is one of 29 PHNs around Australia working to increase the efficiency and effectiveness of primary healthcare and service systems.
It works across the region with general practitioners (GPs), community health, Aboriginal Community Controlled Health Organisations (ACCHOs), pharmacy, aged care and allied health practitioners, and with acute services such as hospitals, specialists and emergency care. The Murray PHN region covers almost 100,000sqkm of regional Victoria.
For more information about the Murray PHN see here.
