There is nuance behind the headlines, and the FSANZ has called for a nationally consistent framework of IVF regulations.
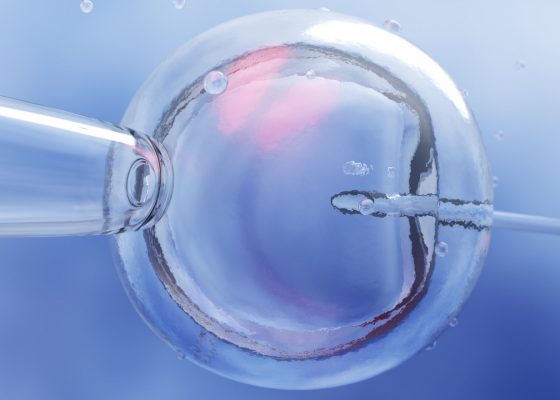
When it comes to fertility treatment, trust is everything. Patients place their hopes, bodies, and futures in the hands of professionals.
That trust must be earned, and continually reinforced, not only through compassion but through clear standards, accountability, and openness.
So, when media reports highlight rare mistakes in IVF clinics, it’s understandable that patients worry. But context matters.
Australia’s fertility care system is one of the safest, most transparent, and tightly regulated in the world. The safeguards in place are robust, continually reviewed, and designed to learn from incidents.
A world-leading system, built from the inside out
Long before IVF was legally regulated in Australia, fertility specialists took it upon themselves to set high standards. In 1986, the Fertility Society of Australia and New Zealand (then the Fertility Society of Australia) established the Reproductive Technology Accreditation Committee (RTAC) – a voluntary, profession-led initiative to safeguard patients and ensure ethical practice.
This wasn’t imposed from above; it came from the clinicians and scientists themselves.
By 2002, that commitment became law. Today, every Australian clinic working with human embryos must be accredited under RTAC’s Code of Practice (here and here). Clinics are audited annually by independent certifying bodies, with inspections covering everything from lab processes to consent protocols.
Clinics can’t just “pass” once and be done – they must demonstrate continuous improvement, year after year.
The purpose of an audit is to proactively identify risks (non-conformances), in order to prevent errors. These non-conformances may be in a clinic’s policies or its procedures or adherenceto policies or procedures. A non-conformance (NCR) is an audit term meaning a deviation from established standards, specifications, or procedures.
Media stories about audit results in RTAC’s annual report for 2023-24 have misrepresented the data. When looking at audit data it’s important to understand that audits are proactive, they are not intended to capture or investigate errors that have occurred, but to prevent them occurring. Importantly, the 2023-24 annual report notes that “all the major NCRs were resolved adequately, and all were associated with a policy or procedure omission”.
What does RTAC’s role include?
Under RTAC’s accreditation system, clinics are held to 15 “critical safety and quality” standards (here and here). These include patient identification, medication management, emergency care access, prevention of ovarian hyperstimulation, and strict protocols to avoid mix-ups of sperm, eggs, or embryos. Every incident or complaint must be logged, investigated, and acted upon.
In addition, clinics must meet 16 “good practice” standards, including having a formal quality management system, providing clear patient information, and safely managing stored embryos and gametes (here and here). These standards are reviewed every three years to reflect advances in science and care.
As part of their responsibilities as a licensed IVF provider, clinics themselves must report events immediately so an investigation can be swiftly initiated. Serious breaches of the code of practice can result in a provider losing its licence.
Related
Behind the headlines
It’s true: rare errors have occurred in IVF labs in Australia. And every one of these cases deserves scrutiny. But headlines can sometimes create the impression of widespread systemic failure. That’s not the reality.
Every incident is investigated under an independent, nationally consistent framework. Serious breaches are exceptionally rare.
Related
Australia also maintains a national IVF outcomes database (ANZARD) that’s among the most comprehensive in the world. Thanks to this data-driven oversight, Australia’s IVF multiple birth rate (a key safety indicator) has fallen to just 2.8%, one of the lowest globally.
Why national consistency matters in fertility care
Even though the clinical standards in IVF clinics are nationally consistent, the laws that govern fertility treatment vary widely across Australia. Each state and territory set its own rules on important issues – like how many families a donor can help create, how long embryos can be stored, and whether surrogacy is legal and accessible.
This patchwork of regulations can lead to confusion, unfair differences in care, and legal grey areas – especially when people, clinicians, or donated materials cross state lines. Patients may unknowingly face different rights or restrictions depending on where they live or where they seek treatment.
That is why the FSANZ is calling for a nationally consistent framework – one that ensures all Australians have access to safe, ethical, and equitable fertility care, no matter their postcode.
FSANZ also supports establishing RTAC as an independent, statutory authority to strengthen oversight and trust, along with a national donor registry to improve transparency and protect donor-conceived individuals and their families.
Transitioning RTAC to an independent body will provide the regulatory authority and operational flexibility needed to uphold rigorous accreditation standards and respond swiftly to emerging risks.
In a climate of heightened public scrutiny and increasing calls for accountability, independence enables RTAC to lead reforms that strengthen confidence in ART services – such as introducing risk-based performance metrics at the clinic level.
This level of transparency is not merely a compliance exercise; it is a cornerstone of safe, high-quality, and person-centred care. It empowers patients, reassures the public, and aligns the fertility sector with the national standards expected across the broader healthcare system.
Transparency builds trust
Fertility care will always carry ethical, medical, and emotional complexities. But what sets Australia apart is a culture of collaboration – between clinicians, scientists, regulators, and patients – to make the system better.
We encourage an industry culture of open disclosure; this is evidenced with reporting of all items of non-conformance – big and small. Any issue is acknowledged, investigated, and used to drive improvement. That’s how trust is earned and sustained.
Looking ahead, national fertility laws, a central donor registry, and an independent RTAC would only strengthen this trust, ensuring that all Australians benefit from the highest standards of care – wherever they live, and whatever their path to parenthood.
Petra Wale is president of the Fertility Society of Australia and New Zealand.